MCCQE1 | CanMEDS Roles

On the journey to becoming a physician in Canada, the Medical Council of Canada Qualifying Examination (MCCQE) Part I is an essential milestone for medical graduates. Passing MCCQE Part 1 successfully requires candidates to possess both medical knowledge and the ability to apply it effectively in the clinical setting.
The Canadian Medical Education Directives for Specialists (CanMEDS) roles are at the heart of understanding and applying medical knowledge. These roles provide an all-encompassing overview of the responsibilities that represent a well-rounded physician. The CanMEDS framework outlines the vital competencies required for every physician, ensuring they practice medicine safely and effectively.
Designed with passion by the Royal College of Physicians and Surgeons of Canada (RCPSC), this groundbreaking framework aims to promote professional medical competencies among Canadian physicians. Its significance has become increasingly important in assessing medical competency, particularly during the MCCQE1 exam.
In this article, we will take a closer look at the history of CanMEDS, its various roles, and how it can help you prepare for the MCCQE1 exam. Whether you are a Canadian medical student or an international medical graduate, understanding CanMEDS is essential to your success in the field and scoring high on the MCCQE1 exam. So, let’s dive into this fascinating topic and discover what CanMEDS offers.
What Does CanMEDS Stand For?
In healthcare, CanMEDS defines the competencies and roles expected of physicians and healthcare professionals. CanMEDS stands for Canadian Medical Education Directives for Specialists and is a framework developed in Canada that has been adopted widely worldwide.
CanMEDS aim to prepare physicians to meet the evolving challenges in healthcare. It involves seven roles that serve as the foundation for the competencies need to for healthcare professionals to provide high-quality patient care.
The Medical Expert role focuses on the clinical skills and knowledge need to for patient care. The Communicator role emphasizes the importance of clear, effective communication with patients, colleagues, and other healthcare professionals. The Collaborator role emphasizes teamwork and promotes that healthcare professionals must collaborate to provide optimal patient care.
The Leader role focuses on developing leadership skills, decision-making, and the ability to manage resources to improve patient care. Health Advocacy addresses social determinants of health and promotes public health policies. The Scholar role emphasizes lifelong learning and unremitting professional development. Finally, the Professional role focuses on maintaining ethical and professional standards and prioritizing patient safety, privacy, and confidentiality.
In order to provide high-quality patient care, the CanMEDS roles emphasize collaboration, communication, lifelong learning, and professional ethics, among other competencies. Implementing CanMEDS has transformed healthcare education, assessment, and practice globally, particularly in Canada.
On the other hand, understanding the significance of the CanMEDS roles in today’s healthcare system is crucial. These roles are not just mere titles but represent the essential skills and competencies that healthcare professionals must possess to provide quality patient care. Later in this blog, I will associate each role with a clinical case and highlight the CanMEDS role’s significance.

What Is The CanMEDS Framework?
The CanMEDS framework is a groundbreaking and transformative approach designed to enhance medical education and improve patient care. Developed by the Royal College of Physicians and Surgeons of Canada, this visionary framework has been adopted across Canada and globally, inspiring healthcare professionals to strive for excellence.
At the heart of the framework lies a core mission: to produce well-rounded physicians who possess clinical expertise and an array of essential competencies vital for delivering holistic and person-centred care. This includes communication, collaboration, leadership, health advocacy, scholarship, and professionalism.
Imagine how an exemplary physician ought to be – one who listens attentively to their patients earns their trust through empathy and compassion and collaborates seamlessly with other healthcare providers in the best interest of the patients they serve. The CanMEDS framework aims to cultivate these qualities in every medical professional.
By incorporating seven key roles – Medical Expert (central role), Communicator, Collaborator, Leader, Health Advocate, Scholar, and Professional –this model fosters a more comprehensive understanding of what it truly means to be a competent physician. It recognizes that for optimal patient outcomes, doctors must go beyond technical skills; they must embrace a multidimensional skillset encompassing emotional intelligence, critical thinking abilities, and ethical values.
The CanMEDS framework has revolutionized medical education by emphasizing that exceptional patient care requires an intricate balance between clinical skills and human connection. As future generations of physicians step into this world guided by these principles, we can expect enhanced collaboration among healthcare teams and improved quality of life for our communities – all thanks to the unwavering passion behind the framework!
Not only that, but the CanMEDS framework plays a key role in the MCCQE1 exam, as it is an examination that assesses the medical knowledge and clinical skills of medical graduates and is also designed to assess a candidate’s communication skills and professionalism, which are essential qualities for any practicing physician.
So, gaining a deep understanding of this framework is crucial for candidates to ensure their utmost preparedness for the exam. This is an incredibly significant aspect because the MCCQE1 exam is a decisive tool that gauges their readiness to practice medicine in Canada’s beautiful and diverse nation.
What Is the History Behind the CanMEDS Role?
The Royal College developed the CanMEDS framework in the 1990s to improve patient care by enriching physician training, and it was formally adopted by the Royal College of Physicians and Surgeons of Canada (RCPSC) in 1996.
The framework is an inspiring and transformative cornerstone of medical education and training in Canada. This holistic approach goes beyond technical expertise by empowering physicians to be well-rounded professionals who make a difference in patients’ lives.
It captures the essence of what it means to provide exceptional care, fostering the development of outstanding doctors with unparalleled competencies across all areas.
Built on a foundation of empathy, passion, and dedication, the CanMEDS framework sparks lifelong learning and continuous improvement among healthcare practitioners. With its focus on collaboration, communication, leadership, and advocacy skills, this framework nurtures remarkable physicians who are compassionate healers as well as advocates for their patients.
Elevating healthcare through innovation and integration, the CanMEDS framework challenges medical professionals to rise above the ordinary and embrace excellence. By cultivating a vibrant community of skilled practitioners adept at navigating complex medical situations with grace and confidence, this framework continues to revolutionize patient care in Canada – one life-changing encounter at a time!
The framework is a globally accepted tool that provides a foundation for understanding the competencies required of physicians. The development of CanMEDS was a collaborative effort, with input from hundreds of Royal College Fellows and volunteers.
One reason for the success of CanMEDS is its commitment to renewal. As medical knowledge advances and clinical practices transform, it is essential for physicians to adapt their competencies accordingly. For this reason, the CanMEDS framework has undergone two significant revisions since its initial introduction – first in 2005 and later in 2015.
These updates serve to maintain the relevance and value of the CanMEDS framework, offering a comprehensive understanding for physicians regarding the necessary skills and expertise to deliver exceptional patient care.
CanMEDS is a vital asset for physicians, playing a crucial role in their practice. Its ongoing evolution, marked by regular updates, guarantees its enduring value as a resource for years to come. Anticipate the release of the next update in 2025, further enhancing its effectiveness and relevance.
The framework consists of seven roles that physicians should embody: Medical Expert, Communicator, Collaborator, Leader, Health Advocate, Scholar, and Professional. Each CanMEDS role is accompanied by a series of competencies that physicians must demonstrate in order to provide high-quality patient care.
In particular, the latest version of the framework – CanMEDS 2015 – places greater emphasis on non-clinical skills such as leadership and teamwork. For example, a new competency in this version is “leader,” which includes team management and decision-making skills.
Another important addition to CanMEDS 2015 is the focus on patient safety and quality improvement. The RCPSC recognizes that physicians play a critical role in promoting patient safety and quality care within their organizations. As such, the updated framework includes competencies related to identifying opportunities for improvement, implementing change, and evaluating outcomes.
However, let us not forget the true purpose of the MCCQE1 exam as you delve into this blog in search of the enigmatic CanMEDS framework and guidance on preparation for the formidable MCCQE Part I exam.
MCCQE1 stands as a formidable gauge of your medical knowledge and clinical skills, meticulously crafted by the Medical Council of Canada to scrutinize the competence of aspiring physicians yearning to practice medicine in Canada. Thus, it’s crucial to dedicate sufficient time and effort to studying and comprehending the material thoroughly.
The exam is an arduous expedition that demands unwavering commitment and steadfast determination from those who wish to conquer it. In your quest for triumph, this humble blog can serve as a beacon, an invaluable companion in your odyssey towards preparation.
This blog serves as a valuable resource to supplement your learning and better prepare you for the MCCQE Part 1 exam. Utilize all available resources, including this blog, to enhance your knowledge and skillset, ensuring that you are fully prepared for success on exam day.
You may encounter a question related to skills in team management and leadership or clinical case on health advocacy. These questions are designed to assess your ability to work collaboratively with other healthcare professionals and make informed decisions in complex clinical situations. It is essential to familiarize yourself with the CanMEDS framework and practice applying it in various scenarios to improve your performance on the MCCQE1 exam.
Overall, the evolution of CanMEDS reflects a growing recognition among medical educators and practitioners that being a good physician requires more than just clinical expertise. By emphasizing non-medical expert roles such as leader and health advocate, the framework encourages physicians to take a more holistic approach to patient care that takes into account not just medical needs but also social determinants of health.
What Are The 7 CanMEDS Roles?
The CanMEDS framework stands at the forefront of medical education, encompassing a range of competencies that are essential for medical practitioners. These competencies go beyond mere knowledge and skills; they contain attitudes and values, fostering a holistic approach to medical training and practice.
The framework addresses physicians’ diverse roles, ensuring they are equipped with the necessary tools to provide exceptional care and positively impact the field of medicine. By emphasizing the seven roles and their corresponding competencies, the CanMEDS framework shapes healthcare professionals into well-rounded individuals capable of meeting the demands of their profession.
CanMEDS Roles | |
Medical Expert | This is the central role in which physicians apply medical knowledge, clinical skills, and professional values to provide patient-centred care. |
Communicator | Physicians communicate effectively with patients, families, and other healthcare professionals to establish relationships and foster therapeutic partnerships. |
Collaborator | Healthcare professionals work together to ensure that patients receive excellent, secure, and efficient care through physician collaboration. |
Leader | Physicians demonstrate leadership in healthcare organizations by promoting safe and efficient patient care, advocating for quality improvement initiatives, and engaging in health policy development. |
Health Advocate | Physicians advocate for their patient’s health needs and contribute to community health initiatives that address social determinants of health. |
Scholar | Physicians engage in lifelong learning and scholarship to maintain competence in medical practice and contribute to advancing knowledge within their field. |
Professional | Physicians uphold high standards of professionalism by demonstrating ethical behaviour, maintaining confidentiality, and reflecting on their practice to improve performance. |
It serves as a guiding light for physicians’ professional development, offering a comprehensive roadmap for growth and excellence. It recognizes the importance of providing medical expertise and effectively communicating with patients, collaborating with multidisciplinary teams, advocating for patients’ rights, embracing lifelong learning, assuming leadership roles, and upholding professionalism.
The CanMEDS framework serves as a crucial pillar in medical education and practice, providing a comprehensive set of competencies that are vital for physicians. While understanding the framework is essential, delving into the fundamental principles behind each role becomes even more valuable when complemented with clinical examples from real-world scenarios.
Moreover, by exploring these examples, aspiring physicians can gain a deeper appreciation of how the CanMEDS competencies manifest in the context of multiple-choice questions and Clinical Decision-Making (CDM) cases, thus enhancing their ability to apply their knowledge effectively.
When it comes to the Medical Council of Canada Qualifying Examination Part 1 preparation, it is paramount to align your study plan with the competencies outlined in the CanMEDS framework. So, you can confidently navigate the exam and demonstrate your readiness to deliver high-quality care to patients, especially in the CDM portion of MCCQE Part 1.
This alignment ensures that you are well-prepared to address the complexities of patient cases and make informed clinical decisions, showcasing your ability to integrate the CanMEDS competencies into your practice.
Let’s examine each role by presenting a clinical scenario and emphasizing their significance for the MCCQE1 exam:
Medical Expert
This role encompasses the knowledge and clinical skills necessary for effective patient care, diagnosis, and treatment. It forms the foundation of the CanMEDS framework, highlighting the importance of medical knowledge as a cornerstone for other roles.
It is the role of a medical expert that truly distinguishes an enthusiastic physician from the rest. To become an expert in the field of medicine, one must possess an unwavering passion for the subject matter. This passion is what drives individuals to seek answers and solutions for every symptom and ailment their patients present.
The journey toward medical expertise begins with a deep hunger for knowledge and understanding. Aspiring physicians must constantly feed this hunger by immersing themselves in continuous learning and skill development. Take, for instance, acute myocardial infarction.
While every medical student learns about this condition, only a few go above and beyond that truly grasp the intricacies of managing an acute MI efficiently and cost-effectively.
The path to expertise in medicine is paved with diligent study and relentless practice. When medical students dedicate themselves to this pursuit, their ability to recall essential information and critical steps in management becomes increasingly robust.
This enhanced recall translates into precision when issuing orders and writing prescriptions, ultimately leading to fewer complications and better patient outcomes.
Now, let’s read a clinical scenario for a medical expert role:
A 65-year-old male presents to the Emergency Department with a sudden onset of severe chest pain radiating to the left arm and jaw. The pain started an hour ago while he was watching television at home. He has no significant medical history but reports occasional episodes of mild chest discomfort, mostly during exercise. Vital Bp160/100 mmHg, HR 100 bpm, RR 22 breaths/min, SpO2 95% and Temp. 37°C. On examination, the patient appears diaphoretic and in moderate distress due to pain. Chest auscultation reveals normal heart sounds without any murmurs or added sounds. Lung fields are clear on auscultation bilaterally.
The role of a medical expert highlights the significance of possessing a robust medical knowledge base and clinical skills that are necessary for diagnosing and managing patients’ health issues. For instance, the vital signs here:
- Blood Pressure: 160/100 mmHg (high)
- Heart Rate: 100 bpm (tachycardia)
- Respiratory Rate: 22 breaths/min (slightly elevated)
Every single one of them tries to tell you something and help you make sound clinical decisions, but if you know about them. Otherwise, for someone without proper knowledge, these numbers do not raise the red fag.
On the other hand, one with a good medical background will realize right off the gate this is a serious medical condition, and time is of the essence; order proper initial laboratory tests, for instance:
- Complete blood count (CBC)
- Basic metabolic panel (BMP)
- Troponin levels
- Electrocardiogram (ECG)
The ECG shows ST-segment elevation in leads II, III, and aVF, suggestive of an inferior ST-elevation myocardial infarction (STEMI).
As the patient’s symptoms, vital signs, physical examination findings, and ECG all point towards an acute coronary event, the medical expert must act quickly to provide appropriate management according to established guidelines for STEMI patients. Start the proper management:
- Administer high-flow oxygen therapy.
- Provide analgesia with intravenous morphine.
- Initiate dual antiplatelet therapy with aspirin and a P2Y12 inhibitor.
- Administer intravenous nitroglycerin for blood pressure control and relief of chest pain.
- Initiate anticoagulation with unfractionated heparin or low-molecular-weight heparin.
The MCCQE Part 1 exam evaluates a candidate’s knowledge and competency in medicine by testing their comprehension of various diseases and management protocols listed in the MCC objectives.
Chest pain is a frequent complaint in medical practice and is an objective number 14 of the Medical Council of Canada (MCC) requires clinicians to differentiate between fatal conditions, such as aortic dissection or myocardial infarction, and less severe causes, like costochondritis or panic attacks.
Understanding chest pain’s causes and potential outcomes is essential for accurate diagnosis and treatment. Adopting a systematic approach for assessing chest pain is crucial, starting with an accurate history and physical examination, followed by appropriate imaging studies if necessary. In addition, pertinent laboratory tests may be employed to aid in identifying the cause of chest pain.
Interestingly, chest pain accounts for over 600,000 visits to emergency departments annually (2018-2019), as per the Canadian Institute for Health Information (CIHI). Furthermore, research published in the Canadian Journal of Cardiology reports that roughly one in five Canadians experience acute chest pain at some point during their lifetime.
Despite being a common presentation in emergency departments, chest pain management frequently lacks proper organization and execution. This raises the possibility of missed diagnoses leading to avoidable morbidity and mortality rates.
This failure to properly manage this condition could lead to a decrease in patient survival rates due to delayed treatment, and given the statistics of chest pain prevalence, the lack of proper ordering of diagnostic procedures could be seen as a huge collective failure since it would be effectively taking away the chance of survival from those in society we are sworn to serve.
This includes recognizing signs and symptoms, assessing patient risk factors, ordering necessary laboratory tests and imaging studies, and initiating necessary treatments as soon as possible.

Communicator
Proper communication skills are paramount in the healthcare industry. The role of communication, as outlined by CanMEDS, encompasses vital characteristics such as empathy, active listening, and clear information exchange.
Empathy is undoubtedly the key to unlocking deeper connections with patients and comprehensively understanding their chief complaints. Active listening enables you to delve into the intricacies of their medical conditions, paving the way for more informed clinical decisions. Yet, among these essential healthcare elements, clear information exchange reigns supreme.
Clear information exchange has the power to dramatically enhance a patient’s comprehension of their own health situation. This fosters improved compliance with treatment plans and ultimately leads to more effective recoveries. Even more importantly, it protects against clinical errors and shields physicians and patients from the daunting prospect of legal battles.
As a physician, you will encounter countless individuals seeking your expertise – on any given day, you might find yourself attending to 20 or 30 patients. With this relentless pace, there is simply no time to hone your communication skills within the confines of the ward.
So, seize every opportunity now to practice explaining complex medical concepts using simple language that anyone can understand. Mastering this skill will not only enhance your ability to convey crucial next steps in a patient’s care but will also solidify your reputation as an exceptional and compassionate healthcare provider. Trust me when I say that you do not have time to practice in the ward.
Physicians equipped with excellent communication skills can effortlessly establish meaningful connections with patients, aiding in comprehending their condition and the rationale behind treatment instructions. This ultimately translates into improved health outcomes for patients.
Now, let’s delve into a clinical scenario:
Mrs. J, a 23-year-old woman, arrived with complaints of lower abdominal pain and vaginal discharge. After conducting a thorough history and physical examination, the physician diagnosed her with pelvic inflammatory disease (PID) and prescribed antibiotics and other medications as part of her treatment plan. But, Mrs. J expressed hesitation in following the prescribed medication regimen due to concerns about potential side effects. Also, she desired more comprehensive information about her condition and alternative treatment options.
Recognizing the pivotal role of effective communication in ensuring Mrs. J receives optimal care, the physician assumed the communication role of CanMEDS. With empathy and clarity, the doctor explained PID to Mrs. J in straightforward terms, encompassing its causes, symptoms, and potential complications if left untreated. Furthermore, the physician discussed the benefits and risks of various treatment options while addressing Mrs. J’s concerns.
Through adept and empathetic communication, the physician skillfully forged a strong rapport with Mrs. J, instilling profound trust and unwavering confidence within her. This conscientious approach notably assuaged her mounting anxiety and alleviated her profound confusion regarding the most appropriate path forward.
As a result, Mrs. J now understands the critical role medication compliance plays in her well-being. Furthermore, she is aware of the potential side effects and complications arising from non-compliance. Equipped with this newfound knowledge, she stands empowered to take proactive measures to avert any future lapses, thereby ensuring a more seamless and harmonious healthcare journey.
It is important to note that PID is a condition frequently caused by sexually transmitted infections, such as chlamydia or gonorrhea, among the young population. The worse thing about it is that if poorly managed due to a lack of compliance, PID can result in serious complications, including ectopic pregnancy, which is a life-threatening condition.
So, effective communication skills are imperative in the healthcare industry when providing patients with information regarding medical conditions like PID. Using simple language and displaying empathy while addressing their concerns will enhance patient compliance with treatment plans and help prevent further complications.

Collaborator
Teamwork is crucial in the healthcare industry for delivering high-quality care effectively. With various healthcare professionals involved, collaboration between disciplines plays a vital role in providing appropriate and efficient medical treatment.
A collaborative environment ensures that all pertinent information is shared among team members to set up the most effective treatment plan for the patient.
Physicians should strive to create such an environment by collaborating with colleagues from different healthcare disciplines. This entails recognizing and appreciating the contributions and expertise of other healthcare professionals.
Let’s read the following clinical scenarios:
A 60-year-old male patient who has a history of hypertension, type 2 diabetes, and hyperlipidemia visited his family physician with complaints of chest pain and shortness of breath. The physician conducted a thorough physical examination and ordered an electrocardiogram (ECG) to provide an accurate diagnosis.
Upon reviewing the ECG results, it was discovered that the patient had ST-segment elevation in leads II, III, and AVF. This finding indicated an inferior myocardial infarction which requires immediate medical attention for proper treatment and management.
The family physician recognizes the need for urgent intervention and activates the hospital’s cardiac catheterization lab. The interventional cardiologist performs percutaneous coronary intervention (PCI), successfully opening the blocked artery. But, during the procedure, the patient develops hypotension, requiring vasopressor support.
Nurse practitioners monitor vital signs while administering medications for blood pressure control. Respiratory therapists provide oxygenation support through ventilator management. Critical care specialists oversee hemodynamic optimization while providing input on further diagnostic testing needs.
The care team consisting of the family physician, interventional cardiologist, nurse practitioners, respiratory therapists, and critical care specialists work collaboratively using their CanMEDS competencies.
The family physician coordinates communication between team members while providing ongoing management of comorbidities. The interventional cardiologist performs PCI while communicating with other team members regarding patient stability and management.
Encouraging and supporting collaboration empowers healthcare professionals to work together to deliver better patient outcomes. In the clinical case, through their collaborative efforts utilizing their CanMEDS competencies, the care team stabilizes the patient’s condition. The patient is discharged five days later, with follow-up appointments arranged by the family physician to ensure ongoing management of his cardiovascular disease.

Leader
As an entrusted head of the medical team, you hold a challenging and critical role in ensuring the provision of quality healthcare services.
You have an important leadership role as a doctor in the healthcare system. This means you need specific skills like making good choices, managing resources, and speaking up for patients and communities. You should give them clear instructions and support to lead your team well.
You’ll need to display excellent communication skills to effectively communicate with patients, their families, and colleagues in the healthcare sector.
Moreover, your leadership skills will be essential in managing healthcare teams to achieve effective patient care outcomes. You’ll need to develop smart strategies that prioritize patient safety while optimizing resources to provide high-quality care.
As a medical team leader, your role is not just about managing resources or making decisions—it goes far beyond that. It requires a profound passion for the well-being of your patients and a burning desire to impact their lives positively.
Complex situations will arise, demanding your unwavering focus and utmost attention. During these moments, your true leadership shines as you gracefully navigate the intricate web of healthcare to ensure the best possible outcomes for those in your care.
Situational awareness becomes your ally, allowing you to see the subtle nuances and changing dynamics in the healthcare landscape. You possess an acute ability to analyze and comprehend the intricacies of each patient’s unique circumstances. Understanding the broader context allows you to tailor your approach and make informed decisions considering the specific needs and challenges.
Critical thinking becomes your trusted companion, guiding you through the labyrinth of medical dilemmas. But it is an enthusiasm that ignites your every action, a fire that fuels your tireless dedication.
Let’s read the following clinical scenarios:
A 51-year-old patient was admitted to the hospital with severe abdominal pain, vomiting, and fever. The initial assessment revealed that the patient had acute cholangitis and required immediate surgery to relieve biliary obstruction.
The surgeon spoke with the anesthesiologist to outline the anesthesia strategy for the patient. Nonetheless, during the preoperative assessment, they found that the patient had experienced serious allergic reactions to several frequently utilized anesthetic medications.
As a team leader fulfilling the CanMEDS Leader Role, the surgeon had to make prompt decisions regarding the patient’s care. She quickly assessed the situation and identified two options: delay surgery until safer anesthesia options could be identified or proceed with surgery and closely monitor for any adverse reactions.
After discussing these options with her team members, including nursing staff and residents, she decided to proceed with surgery but modified the anesthesia plan by selecting drugs that were less likely to cause allergic reactions. She ensured that all necessary precautions were taken, such as having emergency medications and equipment readily available in case of anaphylaxis (a severe allergic reaction).
The patient underwent successful surgery without any complications related to anesthesia. The surgeon closely monitored the patient’s recovery and ensured timely follow-up care.
In this case, the surgeon demonstrated effective leadership skills by making timely decisions in a complex situation when faced with unexpected challenges. By utilizing her knowledge of medical protocols and expertise in communication and collaboration with other healthcare professionals, she successfully provided optimal care for her patient despite significant risk factors.
As such, this clinical case exemplifies how fulfilling the CanMEDS Leader Role is essential in delivering high-quality healthcare services.

Health Advocate
The health advocate role is a critical component of a physician’s responsibilities. It acknowledges the significance of physicians as catalysts for change in advancing health and advocating for the welfare of their patients and communities. This responsibility extends beyond providing care to individual patients and involves a more comprehensive comprehension of the factors that influence health and issues surrounding social justice.
As essential healthcare professionals, physicians have a crucial role in championing health and safeguarding against diseases. Beyond their fundamental responsibilities of diagnosing and treating ailments, physicians serve as staunch advocates for their patients and communities.
They guide individuals towards making healthy lifestyle choices and embracing preventive measures like vaccinations and screenings. By actively promoting health promotion and disease prevention strategies, physicians contribute to cultivating a culture of well-being that empowers individuals to assume control over their health.
On the other hand, physicians in the health advocate role engage in policy development and influence healthcare systems. They use their expertise to provide evidence-based recommendations for health policy reforms, contribute to the development of guidelines and protocols, and participate in professional organizations that advocate for improvements in healthcare delivery.
The following is a clinical scenario that highlights the role of health advocates according to CanMEDS:
Mr. Johnson is a 55-year-old two decades factory worker who comes to the clinic complaining of persistent fatigue, difficulty losing weight, and increasing blood pressure readings. He has a history of type 2 diabetes and hypertension, both of which are poorly controlled. Despite receiving medications for these conditions, Mr. Johnson’s overall health is declining, and he is at risk of developing further complications.
As a health advocate, your vital responsibility involves recognizing and tackling the social, economic, and ecological elements that lead to Mr. Johnson’s unfavourable health results. Your goal is to promote equity, empower the patient, and advocate for resources and support systems that will improve his health and well-being by:
- Assessing Social Determinants of Health
- Engaging in Shared Decision-Making
- Providing Health Education
- Advocating for Resources
- Addressing Health Inequities
- Follow-Up and Monitoring
Perform a thorough evaluation of Mr. Johnson’s social determinants of health, encompassing his socioeconomic status, living conditions, education, employment, and support networks. Determine any obstacles that could hinder his ability to obtain healthcare services, make healthy lifestyle choices, or comply with his treatment regimen.
Collaborate with Mr. Johnson to understand his personal health goals, preferences, and values. Utilize shared decision-making techniques to ensure his active involvement in decisions regarding his care. Empower him to take ownership of his health and participate in self-management.
Develop tailored health education materials and counselling sessions to improve Mr. Johnson’s understanding of his conditions, their associated risks, and the importance of adherence to treatment. Address any misconceptions and provide practical strategies for managing his diabetes, hypertension, and weight.
Mr. Johnson’s persistent health issues necessitate the identification and linkage to suitable community resources like affordable clinics, nutrition initiatives, and monetary aid. Collaborating with social workers, local organizations, and healthcare professionals is vital for guaranteeing he obtains the required assistance to surmount obstacles to ideal health.
Moreover, it is crucial to acknowledge and tackle any health inequalities experienced by Mr. Johnson because of his low-income level and restricted education. Advocating for policies and efforts that support health equity, diminish disparities, and offer reasonably priced access to healthcare and healthy lifestyle opportunities is essential.
Physicians care beyond clinical interventions and can significantly contribute to improving patients’ health outcomes and overall quality of life by recognizing and addressing the social determinants of health, advocating for resources, and empowering them to take control of patient well-being.

Scholar
The Scholar role is an essential facet of the CanMEDS framework, which highlights the significance of physicians’ role in continuously expanding their knowledge and skills for the provision of excellent patient care. This involves demonstrating a commitment to lifelong learning, which encompasses ongoing professional development and keeping up-to-date with new research findings.
Furthermore, it is necessary to appraise and apply scientific evidence while making clinical decisions critically. This helps ensure patients receive the best possible treatment based on the latest research findings, improving their health outcomes.
In addition to this, the Scholar role also involves contributing to new knowledge through research and innovation. Physicians are encouraged to participate in research activities, which is very easy nowadays with the possibility of online meetings.
It’s truly incredible how technology has enabled us to connect with people worldwide and collaborate on important projects like medical research. With these advancements, physicians are no longer limited by geographic boundaries and can work together seamlessly, regardless of distance.
Consequently, physicians now possess an expanded array of possibilities for contributing their expertise and know-how to worldwide health initiatives without the need for extensive travel planning or participating in in-person gatherings.
However, the best thing about the scholar role is that part where attend (expert physicians) share knowledge and expertise with trainees (medical residents). This is extremely crucial and significantly helps improve healthcare delivery systems to the community as it will increase the precision of young fellows.
Engaging in reflective practice is a critical component of being a scholar. This practice allows physicians to regularly assess their performance, identify areas where they need improvement, and enhance their skills further.
Hospital departments come alive each morning with gatherings and reports, a crucial time when the entire team unites to review the day’s schedule and deliberate on any incidents that have transpired in the ward. These meetings serve as a platform for senior members to critically examine patient management strategies, dissect complex situations, identify improvement areas, and impart invaluable guidance to prevent similar occurrences in the future.
This meeting also paves the way for research opportunities and coveted fellowship positions. Senior physicians, driven by an unwavering commitment to enhancing community healthcare, engage with eager senior residents and share their wealth of knowledge with them. In doing so, they nurture the next generation of medical experts who will continue to uphold the highest standards of care.
Entrusted with selecting dedicated team members for research initiatives, these senior physicians collaborate closely with department heads in envisioning novel research studies. Through this collective effort fueled by passion and ambition, they embark on a journey into uncharted territory, striving to uncover hidden potentials and breakthrough discoveries.
In essence, these morning meetings are more than just routine check-ins—they are dynamic melting pots of conversation where experience meets enthusiasm, ideas transform into innovations, and compassionate caregivers come together as one unstoppable force dedicated to improving patient outcomes.
Let’s read a clinical case for the scholar role of CanMEDS:
Mrs. Smith is a 45 years old, Computer programmer who comes to the clinic complaining of increased thirst, frequent urination, and unexplained weight loss over the past two months. Physical examination findings are Bp 140/90 mmHg, HR 85 bpm, RR 16 breaths/min and BMI 36. His Past Medical History (PMH) reveals a family history of type 2 diabetes mellitus (T2DM) and hypertension. He is a non-smoker and consumes alcohol occasionally. He has no known drug allergies. His laboratory results show a fasting plasma glucose level 190 mg/dL and HbA1c level 8.5%.
Based on the chief complaint, medical history, physical examination findings, and laboratory results, the patient is diagnosed with type 2 diabetes mellitus.
The physician in charge meticulously examines the most recent T2DM management guidelines and recommendations from esteemed sources, such as the Canadian Diabetes Association, with a fervent commitment to providing top-notch educational materials for his patient.
With great care and empathy, the physician elucidates to the patient what T2DM entails and how their laboratory results illuminate the situation and compassionately shares the diagnosis. The physician then passionately expounds on the crucial role of lifestyle modifications (dietary changes, exercise), drawing from evidence-based medicine, while presenting an array of therapeutic options for diabetes, including groundbreaking and highly promising medications currently available.
By supplying comprehensive information about these diverse therapeutic options, the physician ardently empowers the patient to decide which treatment best aligns with their needs and preferences.
Later, always with the patient’s consent, the physician enthusiastically shares personal data collected from treating numerous diabetic patients according to evidence-based guidelines and emerging T2DM therapies. This valuable knowledge is imparted to colleagues, residents or medical students within your clinical setting.
The Scholar Role of the CanMEDS Framework highlights the importance of reviewing cutting-edge guidelines so physicians can stay well-informed about new medications and their effectiveness in managing specific medical conditions. It also emphasizes sharing this vital knowledge regarding evidence-based guidelines and emerging therapies for T2DM with peers in a clinical setting.
With great dedication, the physician engages in thoughtful discussions about advances in T2DM management and prevention strategies with colleagues, residents or medical students. This ensures they are all up-to-date with significant advancements in T2DM management techniques and prevention approaches so they can collectively provide optimal care for patients facing similar health challenges.
In this scenario, the physician demonstrated a high level of professionalism by seeking Mrs. Smith’s consent before sharing any of her personal medical information with the medical residents. This shows that the physician respected Mrs. Smith’s privacy and recognized the importance of informed consent in patient care.
Moreover, by discussing the new guidelines for proper medical condition management with the medical residents, the physician exhibited a commitment to staying up-to-date on best practices and providing quality care to all patients. This not only benefits Mrs. Smith but also has positive implications for future patients who may have similar medical conditions.
The physician’s actions were nothing short of inspiring, showcasing an unwavering commitment to patient-centred care and a relentless pursuit of excellence in healthcare practices. In their role as a scholar, the physician demonstrated exceptional dedication to ensuring that Mrs. Smith received cutting-edge, evidence-based care in accordance with current best practices while remaining vigilant to any novel advancements in her condition or treatment options.

Professional
Professionalism is a vital component of the CanMEDS framework for physicians. It encompasses a broad range of maintaining positive relationships with colleagues, medical residents and other healthcare professionals.
One of the most critical aspects of professionalism is upholding the highest standards of conduct, honesty, integrity, and accountability in all interactions with patients, colleagues, and other healthcare professionals.
Maintaining appropriate boundaries in professional relationships is another core competency related to professionalism. Physicians must understand how to establish and maintain appropriate relationships with their patients while avoiding any conflicts or misunderstandings that could undermine trust and compromise patient care.
Another demanding aspect of professionalism is displaying dedication to continuous self-development. As medical advancements progress rapidly, it is crucial for doctors to stay informed about the most recent technological innovations and best practices.
One of the most prominent examples of the impact of technology in recent times has been the virtual doctor-patient meeting during the COVID-19 pandemic. While younger physicians may have had an easier time adapting to these new modes of communication, many older physicians initially struggled with the technical requirements and had difficulties coordinating with departmental support teams.
However, as the pandemic persisted and remote methods became increasingly necessary, even those who were initially hesitant eventually joined their colleagues in the virtual world. This shift highlights how technology is transforming traditional practices and forcing professionals across all industries to adapt and embrace new tools in order to maintain relevance and provide high-quality service.
Advocating for patients’ needs within the healthcare system as a whole is also an important responsibility that falls under the umbrella of professionalism.
Let’s read a clinical scenario for the Professionalism role:
Mr. B is a 50-year-old man with a history of heavy alcohol use who presents to the emergency department (ED) with severe abdominal pain and jaundice. The ED physician suspects acute pancreatitis and admits Mr. B to the hospital for further evaluation and treatment. Mr. B’s condition worsens during his hospital stay, and he develops complications such as renal failure and respiratory distress. The healthcare team realizes that Mr. B’s alcohol use disorder is complicating his medical management, but they encounter resistance from Mr. B when discussing the need for addiction treatment.
The healthcare team demonstrates professionalism by approaching Mr. B with empathy and compassion while still advocating for his best interests. The doctor discusses the connection between consuming alcohol and acute pancreatitis, as well as the benefit of treatment for alcoholism.
The physician also teamed up with an addiction centre, psychiatrists, social workers, and case managers to develop a comprehensive treatment plan tailored to Mr. B’s specific needs and preferences.
Through these actions, the healthcare team exemplifies the role of professionalism in CanMED by demonstrating effective communication skills, cultural sensitivity, ethical decision-making, collaboration with colleagues, respect for patient autonomy, commitment to patient-centred care, self-awareness of their own biases and limitations in addressing substance use disorders, and ongoing learning about addiction medicine best practices.

What Is the Role of CanMEDS in MCCQE Part 1?
In the dynamic world of medicine, knowledge and clinical skills are often considered the most crucial components needed for medical practice. However, another vital aspect is often overlooked – a set of professional qualities that healthcare providers must possess to provide patients with optimal care.
The CanMEDS framework is designed to ensure that medical professionals are equipped with essential competencies to practice effectively within Canada’s healthcare system. The CanMEDS framework comprises seven roles which include: Medical Expert, Communicator, Collaborator, Manager, Health Advocate, Scholar and Professional.
Within this framework, the MCCQE1 exam assesses a candidate’s readiness to practice medicine effectively within Canada’s healthcare system. The exam evaluates a candidate’s competency level in each domain through various assessment methods, such as written and objective structured clinical examinations.
On the other hand, the Medical Council of Canada (MCC) wholeheartedly embraces the principles outlined in CanMEDS. Indeed, the undeniable link between the CanMEDS roles and the MCCQE1 exam continues to strengthen, particularly in light of recent MCC objectives updates.
For those striving for success on their MCCQE1 exams, a deep understanding of CanMEDS is absolutely crucial. Familiarity with these roles not only illuminates the pathway towards comprehensive coverage of exam objectives but also inspires a fervent passion for excellence within candidates – a passion that will undoubtedly serve them well throughout their medical careers!
Embrace your journey towards mastery with unbridled enthusiasm, and let CanMEDS be your guiding star as you navigate the ever-evolving landscape of healthcare!
Let’s explore the impact of the CanMEDS in MCCQE1 and how it shapes the landscape of medical practice in Canada.
How Does Ace QBank Help with MCCQE1 Exam Preparation?
Proper preparation is essential for success on the MCCQE1 exam. You should make every effort to earn the maximum possible score on the MCCQE1 exam and, importantly, pass the exam on the first attempt.
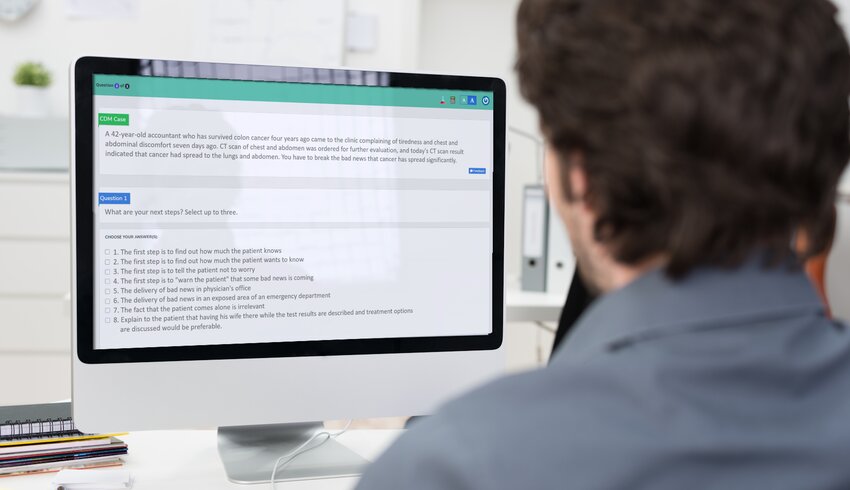
The MCCQE Part I exam is based on the MCC objectives and in accordance with CanMEDS. The most effective method of MCCQE1 exam preparation is to use a question bank to cover the MCC objectives properly.
Ace Qbankis the number one question bank and the best choice for MCCQE1 exam questions that help you cover all MCC objectives with high-yield questions. Proper programming, coverage, and proper testing will guarantee good results.
Ace Qbank is the only Canada question bank designed based on the Medical Council of Canada objectives and has over 2,500 questions designed to prepare you for the first part of the exam, 140 Clinical Decision-Making (CDM) cases for the second part of the exam and two self-assessments to assess your readiness before you it for the exam.
The high-yield quality questions, many summary tables, outstanding flowcharts, detailed explanations for all question options, and top-notch clinical decision-making (CDM) distinguishes the Ace Qbank and makes it the number one question bank for the MCCQE1 exam in Canada.
The questions will be challenging since the MCCQE1 exam is clinically oriented. So, an in-depth explanation of the correct and wrong answers, flowcharts and summary tables will help in answering the exam questions.
Ace Qbank is a one-stop shop. The question bank has over 2400 multiple-choice questions for the first part of the exam, 140 CDM cases for the second part of the exam, and two self-assessments to assess your readiness before you it for the exam.
We invite you to sign up for the Ace Qbank demo today and see the difference our elite question bank makes!