Aortic aneurysm screening Guideline-2021
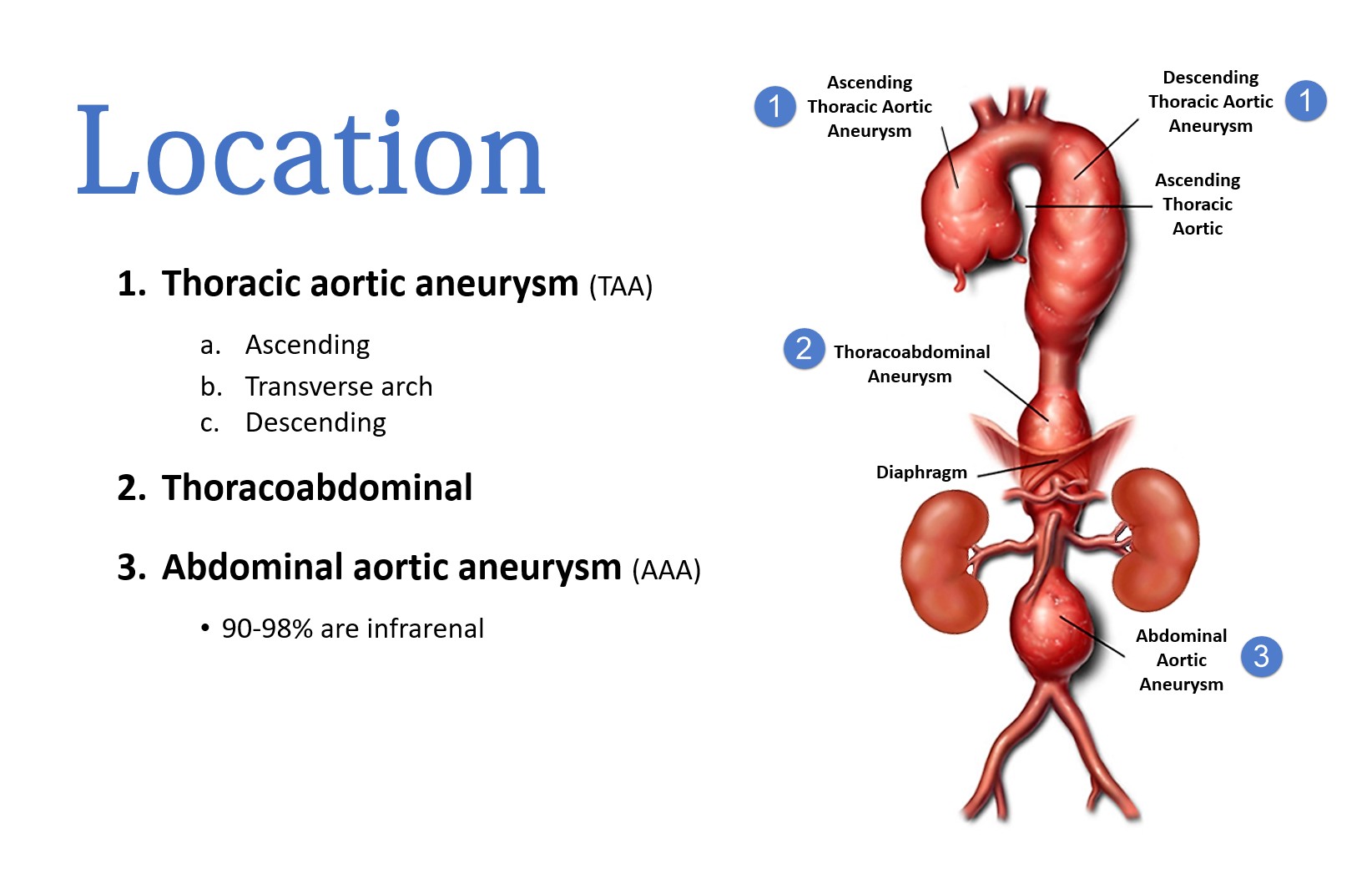
Aortic aneurysm is defined as a permanent, localized dilatation of the aorta to a diameter that is at least 50% greater than is normal at that anatomic level. For most adults, an aortic diameter >3.0 cm is generally considered aneurysmal.
The clinical progression of an aortic aneurysm is continued expansion and eventual dissection or rupture. Hence, regular noninvasive imaging studies, as part of a lifelong surveillance plan, are necessary to ensure long-term patient health. Even small asymptomatic aneurysms should be routinely imaged to assess overall size and yearly rate of expansion.
This article we will briefly review abdominal aortic aneurysm pathology, risk factors, clinical presentation and diagnosis then go through Canadian recommendation and guideline for screening for AAA apply to help standardize the decision-making process for asymptomatic adults aged 65 years and older.
Pathology:
Aortic aneurysms can be either “true” or “false.”
True aneurysms can take two forms: fusiform and saccular.
- Fusiform aneurysms are more common and can be described as symmetrical dilatations of the aorta.
- Saccular aneurysms are localized outpouchings of the aorta.
Abdominal aortic aneurysm (AAA) is the most common true arterial aneurysm.
False aneurysms, also called pseudoaneurysms, are leaks in the aortic wall that are contained by the outer layer of the aorta and/or the periaortic tissue; they are caused by disruption of the aortic wall and lead blood to collect in pouches of fibrotic tissue.
Risk factors:
It is estimated that each year 20,000 Canadians are diagnosed with an AAA and that 1,244 die from an AAA. The important risk factors for the development of abdominal aortic aneurysm (AAA) include:
- Older age
- Male gender
- Cigarette smoking
- Atherosclerosis
- Hypertension
- Family history
- Presence of other large artery aneurysms (eg, iliac, femoral, popliteal)
Male sex is an important risk factor for development of AAAs; the prevalence of AAA among men aged 65 to 80 is 4 to 6 times higher than in women of the same age.
Smokers have a higher risk of AAA. Smoking is associated with formation as well as dilation and rupture of AAAs. Following information are critical in history taking:
- Smoking cessation (current smokers have a higher risk of developing AAA)
- Number of cigarettes/day (>20 cigarettes /day have a higher risk of AAA)
Clinical presentation:
AAA does not typically cause symptoms unless the aneurysm is expanding rapidly, has become large enough to compress surrounding structures and often discovered on either abdominal examination or a radiologic study done for another reason, but abdominal aneurysms may result in abdominal or lower back pain or sense of abdominal pulsation.
Diagnosis:
A definitive diagnosis requires abdominal imaging studies that demonstrate an aortic dilation meeting the criteria for aneurysm. Abdominal ultrasound and computed tomography of the abdomen are both highly sensitive and specific for diagnosing AAA. However, depending upon the presence of symptoms and the hemodynamic status of the patient they are recommended.
Canadian Society of Vascular Surgery 2018 AAA Screening Guidelines Recommend:
One time screening ultrasound for:
- Men age 65-80
- Women age 65-80 with smoking history or cardiovascular disease
- First degree relatives after age 55
Repeat ultrasound 10 year after initial screening if aortic diameter >2.5 cm and <3cm
At Ace Qbank, we work hard to maintain the content up to date and in accordance with medical standards of care. We evaluate the question bank on a regular basis based on current guidelines and recommendations, and we implement any changes we make as soon as possible to enhance your learning experience.
Read more here!
Try Ace Qbank out today!